Is Your Prior Authorization as Pain-Free as Your Patients?

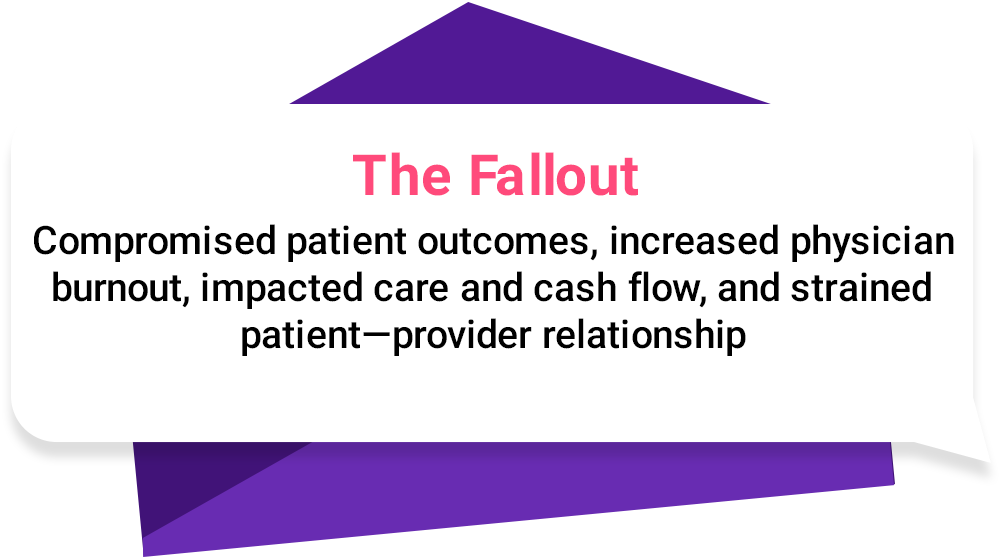
Who would have thought that a simple cost-control measure by health plans could turn into a choke point, becoming a barrier to care and a double whammy for its key stakeholders—patients and providers?
From delaying critical treatments and exacerbating medical conditions of patients to impacting physician utilization and their reimbursements, the ripple effects of prior authorization are far-reaching and devastating, to say the least.
The urgency to fix this broken system has never been greater, and the 2023 AMA prior authorization physician survey says it all.
A Nightmare for Patients and Providers
Hindered Patient Care
94%
78%
24%
12 hrs/week
27%
95%
Why Pain Management Practices Struggle with Prior Authorization
Providers are often boggled down by extensive, non-standard documentation requirements by payers.
Clinical Necessity vs. What’s
Billable
Higher turnaround times (TAT) in payer approvals and frequent denials as a result of excessive scrutiny by payers due to nature of the specialty and its use of opioid therapies result in unnecessary delays in critical, time-sensitive treatments.
But There’s a Remedy to the Prior Auth Pain
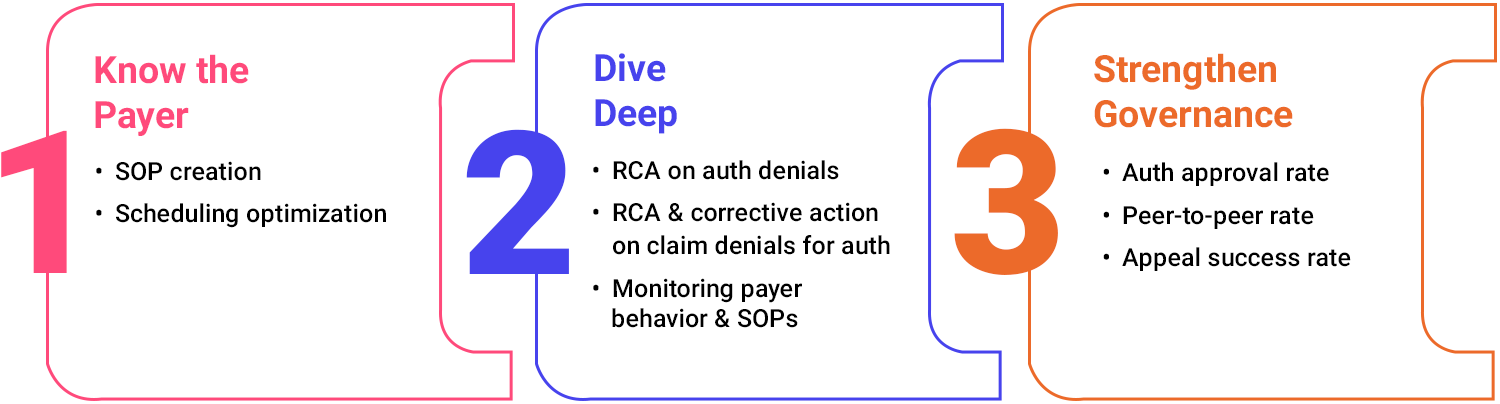
Fortifying Front-End Processes
Appraising and Optimizing Workflows
Tracking and
Governance
How Jindal Healthcare Simplifies Prior Authorization for Providers

At Jindal Healthcare, we empower pain management practices to tackle prior authorization head-on by leveraging our tech-enabled expertise for workflow optimization.
SOP-Driven Documentation Precision

Denial Defense Done Right with RCA and Feedback

KPI-Focused Revenue Cycle Governance

SOP-Driven Documentation Precision

Denial Defense Done Right with RCA and Feedback

KPI-Focused Revenue Cycle Governance
What Sets Us Apart
35%
Increase in
Average Revenue
92%
Authorization
Approval Rate
50%
Reduction in
RCM Costs
Simplify Prior Authorization with Jindal Healthcare for Seamless Patient Access
To explore our full suite of AI-powered RCM solutions, visit www.jindalhc.com.





