REVENUE CYCLE
MANAGEMENT
KNOWLEDGE CENTRE
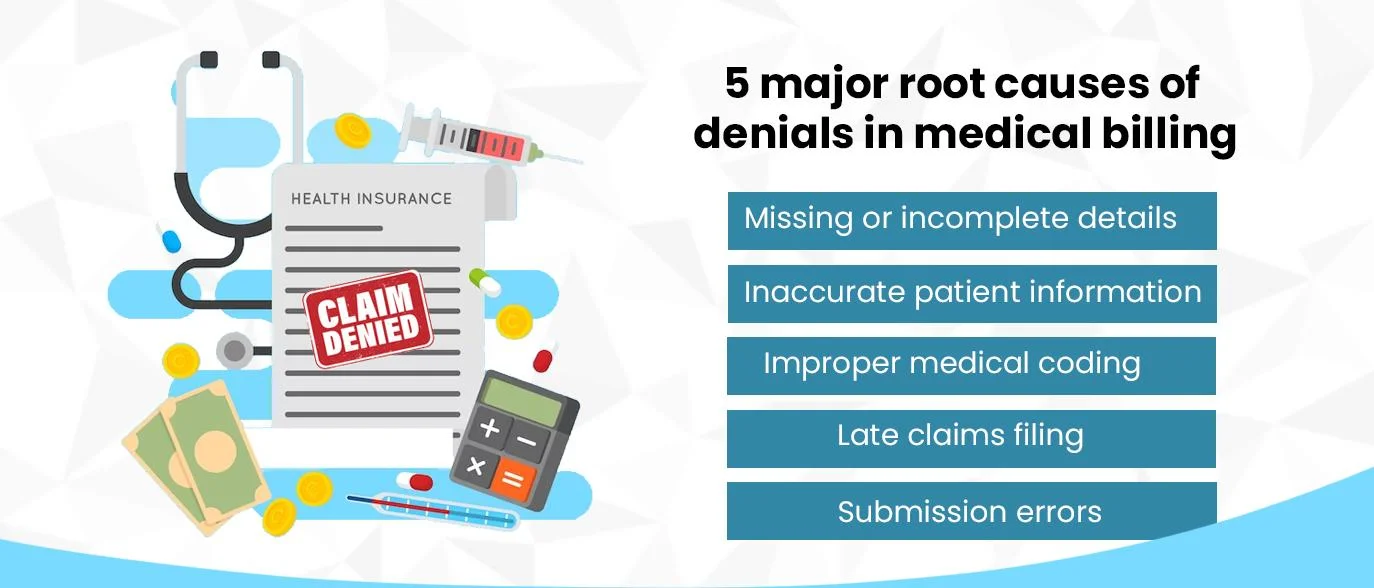
The Data Is Telling: Manual Eligibility Is Breaking DME Revenue Cycles Study after study tells the same story: 30–40% of claim denials stem from eligibility or registration errors, making them the #1 avoidable source of revenue loss every year. And…
Prior authorization (PA) involves getting timely approval from a patient’s insurance firm before providing any service or medication. Navigating through the challenges and administrative burden of this process is easier said than done. According to AMA prior authorization physician survey,…
With the healthcare industry becoming more complicated, traditional methods of revenue cycle management (RCM) are now found incapable of meeting organizational needs. This is resulting in several problems including billing errors, hefty inefficiencies, longer revenue cycles, and significant revenue losses—all…
Delayed revenue collections have now become common in healthcare operations, and we cannot overlook the significant cash flow problems they cause. This can be due to the huge volume of claims involved in medical accounts receivable (AR).In such a scenario,…
The buzz around artificial intelligence (AI) and its evolving applications in the healthcare revenue cycle management (RCM) space refuses to abate, and rightly so! AI’s incredible potential in simplifying revenue cycle operations through automation, actionable insights, and optimized workflows contested…
The dynamic healthcare industry demands healthcare providers to be on their toes, more so when it comes to ensuring they are paid fairly for the services they deliver and the claims they accurately file. Ensuring a steady flow of cash…
The "National Hospital Flash Report: April 2023" indicates that US healthcare providers are struggling with more denials of claims. This problem influences patient treatment and happiness in addition to the financial viability of healthcare companies. Healthcare Denial Management providers have…
According to a recent report from MarketsandMarkets, the global RCM market has been estimated to be worth $49.6 Billion in 2023. And it is expected to attain $84.1 billion by 2028. So, you can understand the value of its market.…
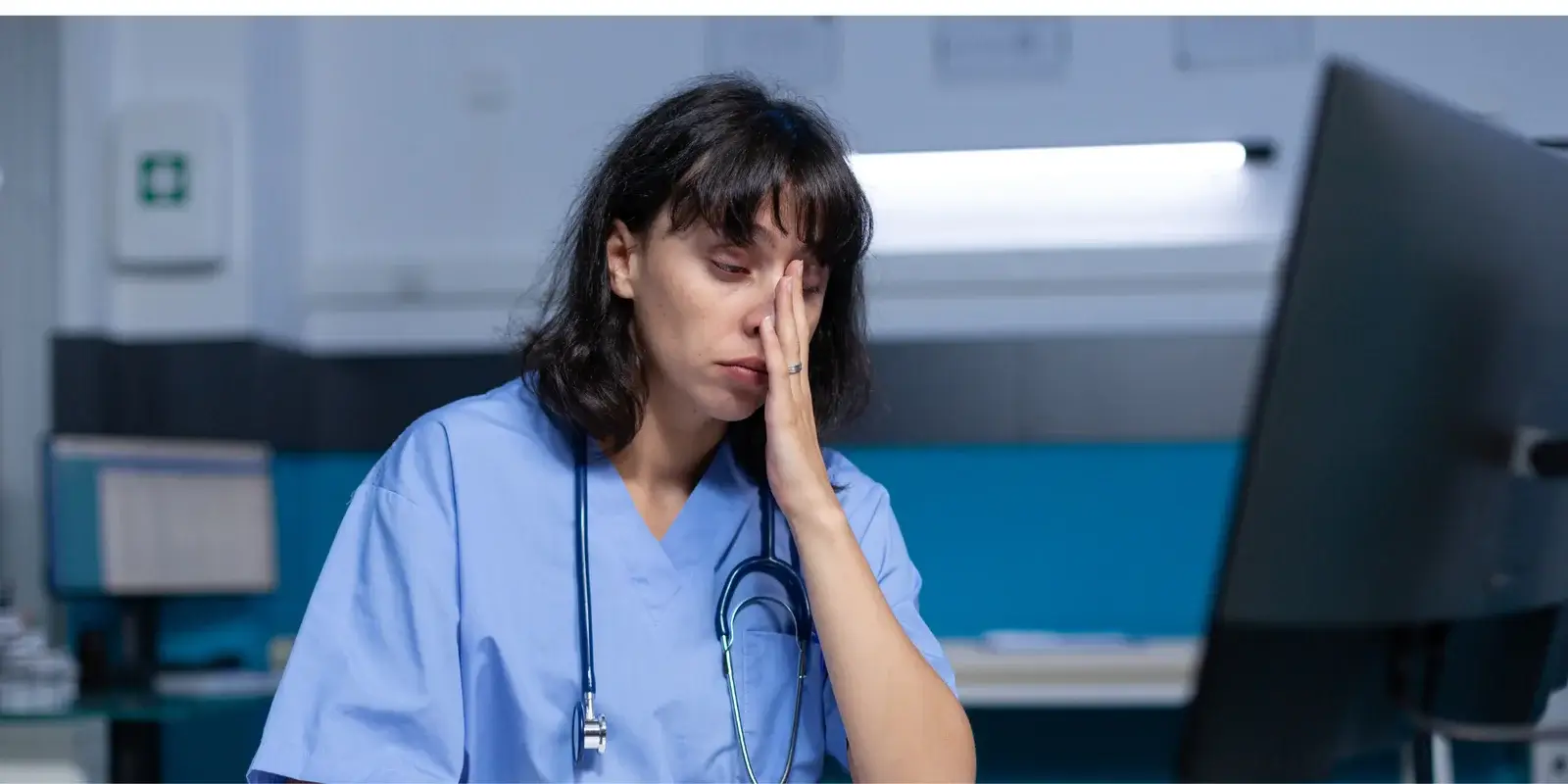
In the ever-evolving healthcare landscape, claim denials often become a thorn in the side of providers and physician practices, costing them financially and draining them physically and mentally. Changing payer behavior and growing staff shortages and burnout further add to…
Claim denials continue to be one of the most dreaded setbacks for healthcare providers, tormenting their revenue cycle and costing them a staggering $20 billion every year. With around $43.84 as the average cost of fighting a claim, the stakes…
Efficient healthcare begins with streamlined workflows. With optimized processes, providers can hit their stride, improving patient satisfaction and maintaining optimal cash flow for better care delivery and service expansion. However, today’s healthcare is mired in complex regulatory and payer policies,…
The 2023 American Medical Association (AMA) prior authorization physician survey is a wake-up call for the healthcare industry, given its telling facts. The nationwide survey of 1,000 practicing physicians reported: Around 94% of respondents citing pre-authorization resulting in care delays About 95%…
The advent of artificial intelligence (AI) has revolutionized the industrial landscape globally, and healthcare is no exception. The much-sought-after technology it is today has long evolved from traditional data analysis to more sophisticated, advanced systems smart enough to optimize patient…
Given the mounting healthcare revenue cycle management (RCM) complexities amid staffing shortages, providers are walking a tightrope and reeling under the constant pressure of delivering high-quality care with limited resources. While doing so, they are also expected to handle claim…
Improving revenue cycle resilience with a clean claim rate requires healthcare systems to implement a well-thought-out strategy that can target denials head-on and help them maintain financial stability in the long run.
Learn how automation revolutionizes eligibility verification in healthcare, improving revenue cycle efficiency, reducing burnout, and enhancing financial performance.
The toll of staff burnout and shortage can be immense on the revenue cycle and patient experience and indeed calls for a pragmatic approach to RCM that focuses on streamlining workflows, mitigating burnout, and improving financial and health outcomes.
Failure to submit the claims within the payers’ timeframe can also result in denials. Outsourcing claim and denial management can prove a game changer in such scenarios for providers lacking the time and resources, ensuring accurate charge capture and timely claim submission.
Reducing accounts receivable days is essential for the success of any medical practice. AR days measure the average time it takes for a claim to be paid, based on the average daily charge volume.
In today's competitive healthcare environment, maintaining accurate and efficient billing practices is crucial for a hospital's financial health.
Effective revenue cycle management (RCM) is vital in healthcare financing as it oversees the entire patient journey from scheduling to final payment and any mistakes in this process can significantly impact healthcare providers' financial sustainability.
Maximizing revenue is crucial for hospitals to maintain quality patient care and invest in new technologies, especially in today’s competitive healthcare environment. Denials on insurance claims can significantly impact your hospital's financial health.
AI-powered automation is revolutionizing the medical billing process, increasing its speed, accuracy, and error reduction. AI can streamline activities, accelerate the medical billing cycle, and eliminate human error.
As the starting point for all healthcare procedures, patient access has a substantial impact on revenue cycle management.
Prior authorization, also known as pre-authorization, is crucial to medical billing. It guarantees that medical professionals are fairly and effectively compensated for the services and treatments they provide.
The rate at which insurers deny medical claims is quite troubling. The average claim denial rate climbed by 23% over the last four years, a recent investigation found. This results in unpaid services lost or delayed income, and a significant financial hit for medical practices.
When assessing the health of a medical practice, the focus is typically on missed collections at the time of service, frequent denials, inadequate claims administration, and aging patient accounts.
Beyond being a mere chronicle, this analysis serves as a beacon, illuminating pathways for navigating the complex tides of change.
The healthcare industry is undergoing an exemplary transformation, with organizations grappling to optimize their revenue cycles. In this pursuit, decision-makers are faced with a crucial choice: should they manage revenue cycles in-house or leverage the benefits of outsourcing?
In the implication of healthcare administration, outsourcing insurance eligibility verification stands as a pivotal process that can significantly impact the efficiency of claims processing. The accuracy and speed with which eligibility is verified can make or break the revenue cycle for healthcare providers.
According to recent study by Etactics, an estimated 80% of medical bills contain errors, and these discrepancies can significantly impede patients' ability to access timely and affordable healthcare.
Evaluating your practice's financial well-being is a pivotal step toward fostering future growth. By gaining insights into the metrics that influence your revenue cycle, you can proactively enhance your practice's efficiency and financial stability.
Managing bills, insurance claims, and patient records can be a daunting task. In fact, healthcare organizations often process thousands of claims, leading to a high potential for errors and inefficiencies. The good news is that technology is coming to the rescue!
As the healthcare industry undergoes a profound metamorphosis, medical practices find themselves at the crossroads of innovation and adaptation. To thrive in this ever-changing environment, medical practices must not only adapt but...
This term might sound complex, but it's essentially a patient’s first interaction with the healthcare system. Think of it as the front door to the world of healthcare.
The implementation of a streamlined denial management procedure will result in a noticeable decrease in claims being declined, resulting in grater warning potential for healthcare companies.
Effective revenue cycle management (RCM) is important for the financial fitness of healthcare companies.
Learn about interrelated nature between Patient Access Management and Revenue Cycle Management in healthcare, its importance, processes, and the revolutionary influence it has on the healthcare sector.
Learn about different coding methodologies, their unique purposes, and how they collectively contribute to the efficiency, accuracy, and success of the healthcare industry.
Medical coding not only helps in identifying issues related to clinical documentation but also produces clear claims while generating revenue without compromising on quality.
The future of A/R management in healthcare holds promising trends that aim to address existing challenges and improve overall efficiency
Accurate and efficient medical billing is vital for optimizing revenue, reducing claim denials, and ensuring the financial viability of healthcare providers.
Efficient management of accounts receivable (A/R) is an essential aspect of every healthcare practice. The effectiveness with which practices handle receivables has a direct impact on cash flow and, ultimately, financial health.
An effective A/R management ensures that the business receives payment for its services on time, reducing the risk of financial instability.
After the financial struggles many health systems faced in 2022 — with operating margins negative for 11 consecutive months according to Kaufman Hall — the revenue cycle is in the spotlight in 2023. Health system leaders are turning to their revenue cycle experts to shape their overall strategies. To navigate these challenging times and optimize financial performance, healthcare organizations are increasingly recognizing the critical role of revenue cycle management services. RCM services encompass a range of strategies, technologies, and processes aimed at maximizing revenue, improving cash flow, and enhancing operational efficiency throughout the revenue cycle.
Medical billing denial is the biggest stumbling stone in the healthcare revenue cycle. As per Etactics, “In 2021, there were 48.3 million denied claims, accounting for 16.6% of all claims submitted that year.” There can be multiple reasons behind rising claim denials in a practice.
What is your biggest revenue cycle challenge? Is it Prior authorization? Rising claim denials? Staffing Issues? Higher accounts receivable (A/R)? As per the Medical Group Management Association's most recent MGMA Stat poll, of the 825 healthcare leaders surveyed, about 48%…
Excessive revenue leakage poses a severe risk for U.S. healthcare practices presently, many already function on negative margins. A 2018 survey conducted by Fibroblast of C-suite executives in healthcare revealed an alarming rate with which hospitals lose money or fall…
American Academy of Pain Medicine stated that millions suffer from acute or chronic pain every year in the US, and the effects of pain exact a tremendous cost, billions of dollars, each year. As the population ages, these numbers are…
The US government enacted The Patient Protection and Affordable Care Act (ACA), a comprehensive health care reform law, in March 2010 to improve the coverage, delivery system and reduce health care costs. Yet there remained a gap between people with…
Healthcare is transforming right in front of our eyes. The last 12 months have rocked the industry to the core. The ways facilities engage with patients from treatment to payment processing are changing. Pain Management Clinics are at a bigger…
In 2023 it’s harder to find dedicated back-office staff that are willing to stay on for the long haul. The average tenure of back-office staff is lower than its ever been. The constant turnover forces facilites to look at other…
Did you know? Between Dec 2019-2021, the median change in hospital operation margins (without CARES) dropped by 14.7%, while labor expenses per adjusted discharge increased by 26.8%. (Jan 2022 National Hospital Flash Report) It’s difficult to retain staff since “The…
As per the Centers for Disease Control and Prevention (CDC), 6 in 10 adults in the US have a chronic disease. Leading drivers include excessive alcohol use, lack of physical activity, and poor nutrition. While people must quickly adopt healthy…
Physicians are under increased stress to provide timely care. They issue prior authorizations (PA) for treatment without fully assessing the patient’s condition. To address this problem, several states have passed pre-auth reform laws that require physicians to obtain a full…
Whether you belong to a multi-specialty group or run your private practice, it's not easy to maintain a strong revenue cycle. Equifax, a credit agency, recently highlighted in a report that healthcare providers lose $1300 on an average daily due…